WVU research shows mindfulness may improve substance use treatment

Patients receiving medication for opioid use disorder are more likely to complete their treatment programs and have a lower risk of relapse if they participate in mindfulness training, according to a West Virginia University study.
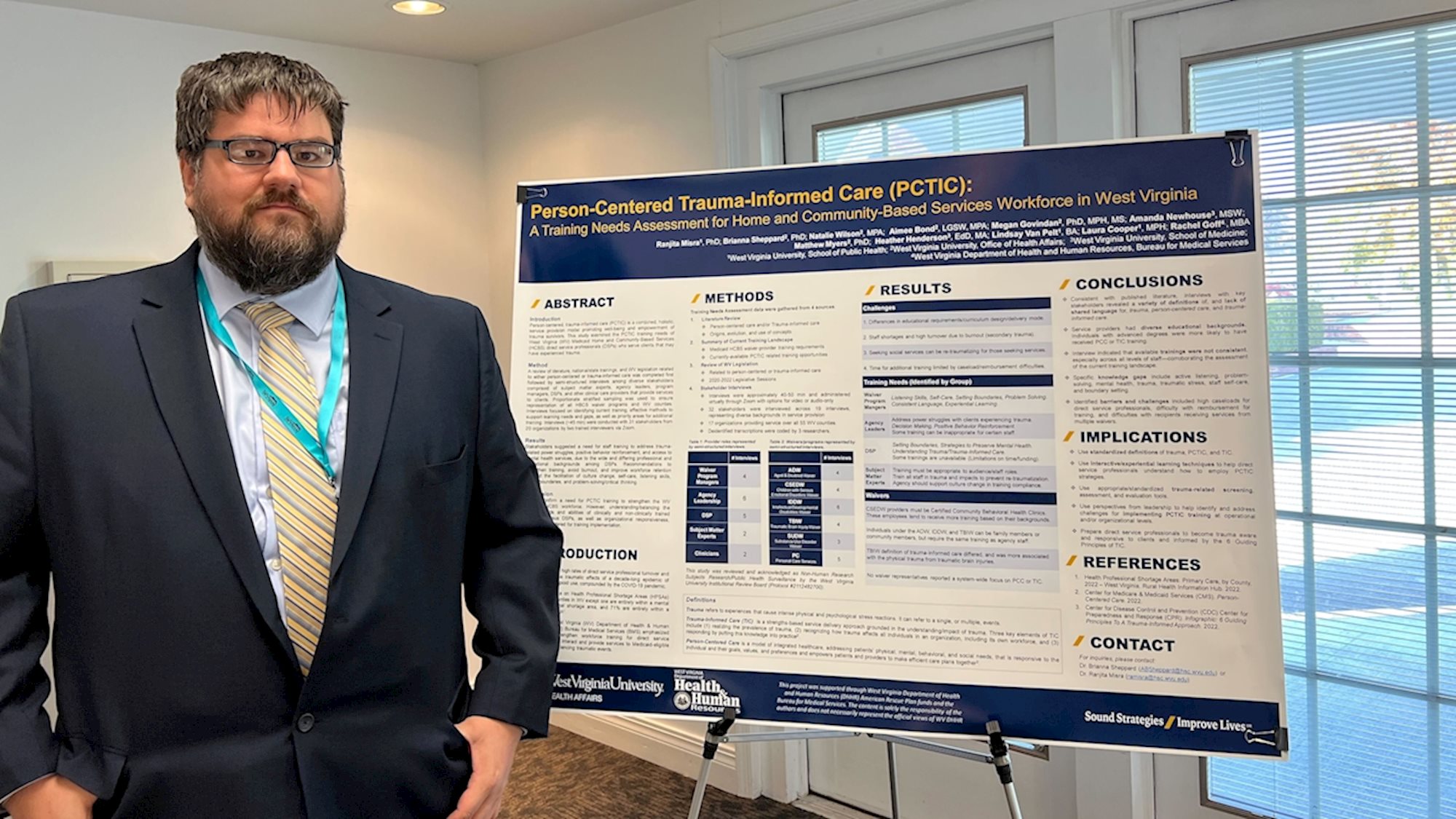
Funded in part by the U.S. Centers for Disease Control and Prevention, the study — led by Johnathan Herczyk, assistant director of program management, risk management and quality assurance at the WVU Health Affairs Institute — was a secondary analysis of data focused on identifying the association between patients’ mental health and retention in a Central Appalachia medication-assisted outpatient treatment program.
An elevated prevalence of depression and anxiety complicates opioid use disorder treatment efforts as does the perception of loneliness, a factor recognized as being directly related to substance use and drug cravings because it increases the risk of mood and anxiety disorders, affects decision making, and influences motivation.
Herczyk’s team aimed to determine if mindfulness — the practice of focusing and being present in the moment — was especially beneficial to patients who perceive loneliness.

Mindfulness may improve a patient’s awareness of internal and external stimuli such as drug use triggers, so they can adapt and recognize them, and have more control of over the outcome, the study found.
“This helps individuals act less on impulse and habit and implement different coping and treatment strategies,” Herczyk said. “Think of mindfulness as a way to help individuals in substance use disorder recovery gradually turn on the lights in a darkened room to notice more of what is going on inside of the room.
The team’s findings suggest mindfulness-based relapse prevention, or MBRP, has potential as a standard-of-care treatment option in pharmacological interventions. Herczyk’s team also plans to further its studies on loneliness and mindfulness in the recovery program setting.
Read more: Mindfulness-based resilience training for frontline workers and first responders
Study participants received care at the WVU Rockefeller Neuroscience Institute Department of Behavioral Medicine and Psychiatry outpatient Comprehensive Opioid Addiction Treatment program. Treatment included biweekly medication management, group therapy and community-based, self-help meetings. MBRP sessions were incorporated into the treatment plan and participants who reported an increased sense of mindfulness were more likely to remain in the program.
“Our team is currently planning to use a mixed methods approach to reevaluate loneliness among this population in a post-pandemic world as well as learn firsthand about the experiences individuals have with loneliness, mindfulness, and stigma during their participation in treatment,” Herczyk said.
“Our hope is to raises awareness of how common this issue is because of its influence with both physical and mental health issues such as cardiac disease, stroke and depression. More specifically though, the hope is that substance use treatment programs begin to consider and address loneliness and isolation among their patients.”
For the study, Herczyk partnered with Keith J. Zullig, Stephen M. Davis, and Danielle M. Davidov, all of the WVU School of Public Health, Jennifer Mallow of the WVU School of Nursing, Laura R. Lander of the WVU School of Medicine, Gerald R. Hobbs, emeritus associate professor in statistics, and Laurie Theeke of George Washington University.
-WVU-
ls/11/15/23
MEDIA CONTACT: Linda Skidmore
Health Research Writer
WVU Research Communications
Linda.Skidmore@hsc.wvu.edu